Medical Innovation: The Path of Prototyping and Certification
Bringing a medical innovation to life is an exciting journey. Every year, innovators dream of creating devices that can improve patient care and transform healthcare. But turning an initial idea into a market-ready medical device requires more than imagination, it requires strategy, planning, and understanding the path from concept to certification. In this article, we’ll explore this journey, highlighting the key milestones, tools, and strategies to turn a concept into a safe, effective, and successful medical device.
Medical innovation starts where and when?
Every medical device begins with an idea, but ideas emerge in many different ways. Some innovations are driven by technology push, when new technical possibilities suddenly open the door to medical applications. Much more often, however, innovation is the result of market pull – the unmet needs of patients that become an urgent call to action. Doctors, surgeons, physical therapists, dentists, and medical caregivers, thanks to their daily contact with patients, are uniquely positioned to see what can be improved to enhance quality of life and standards of care.
Yet not every medical innovation has the potential to grow into a viable solution. At the outset, it is worth asking a few questions:
- What makes an idea different from existing solutions?
- What tangible benefits will it bring to patients?
- How does the competitive landscape look?
Answering these questions early helps ensure that the development process is worth pursuing and that patients and healthcare professionals will ultimately choose your device over others.
Equally important is to clearly define the target group. Health needs vary dramatically between regions. Following WHO and Eurostat data in 2024, an average of 3.8% of people over 16 in the EU reported unmet medical needs, with numbers ranging from 13.4% in Greece to just 0.2% in Cyprus. In countries such as Georgia, Haiti, Morocco, Rwanda, and Zimbabwe, over 50% of individuals aged 60 and above reported unmet healthcare needs in 2023. These figures highlight a crucial truth: a promising medical concept must not only be innovative, but also deeply grounded in the real-world context in which it is intended to operate.
Discover the journey of medical innovation
The Path – From Scratch to a Medical Innovation
You have your medical idea, but now the question is: what milestones lie ahead to turn it into a real medical device? Bringing it to market is far from a sprint – it’s a marathon. Launching a new device can take 3 to 7 years, depending on several factors:
- Device risk class – higher-risk devices face more rigorous and time-consuming development.
- Regulatory pathway – requirements differ across regions (e.g., MDR in Europe, FDA in the US), affecting the timeline.
- Clinical testing – not all devices require clinical trials, low-risk devices may rely on reference data or literature. Finding an appropriate clinical group can be challenging, and trials may last months or even years.
- Regulatory approval – the speed depends on the notified body and target market, sometimes taking up to 24 months.
- Production and market launch – the timeline depends on manufacturing capacity, device complexity, and production volume.
Development can be divided into five key phases, each with its own challenges and opportunities:
- Device discovery and risk analysis – At this stage, you assess potential risks: clinical, technical, and commercial and make sure the medical innovation addresses a real unmet need.
- Formulation, concept and feasibility – Here, you evaluate whether the concept is technically feasible, financially sustainable, and clinically relevant. Early validation is key to avoid investing in unworkable solutions.
- Design and development – verification and validation – Verification ensures the device is built according to the design, while validation confirms it truly meets user needs. Iterations and feedback loops are critical here.
- Final validation and product launch preparation – Aligning evidence, regulatory requirements, and market strategy. Planning early for regulatory approval reduces surprises and accelerates time to market.
- Production, market introduction and post-market follow-up – Launch is just the beginning. Post-market surveillance, user feedback, and iterative improvements often determine whether the device thrives in real-world conditions.
The Role of Prototyping in Medical Device Development
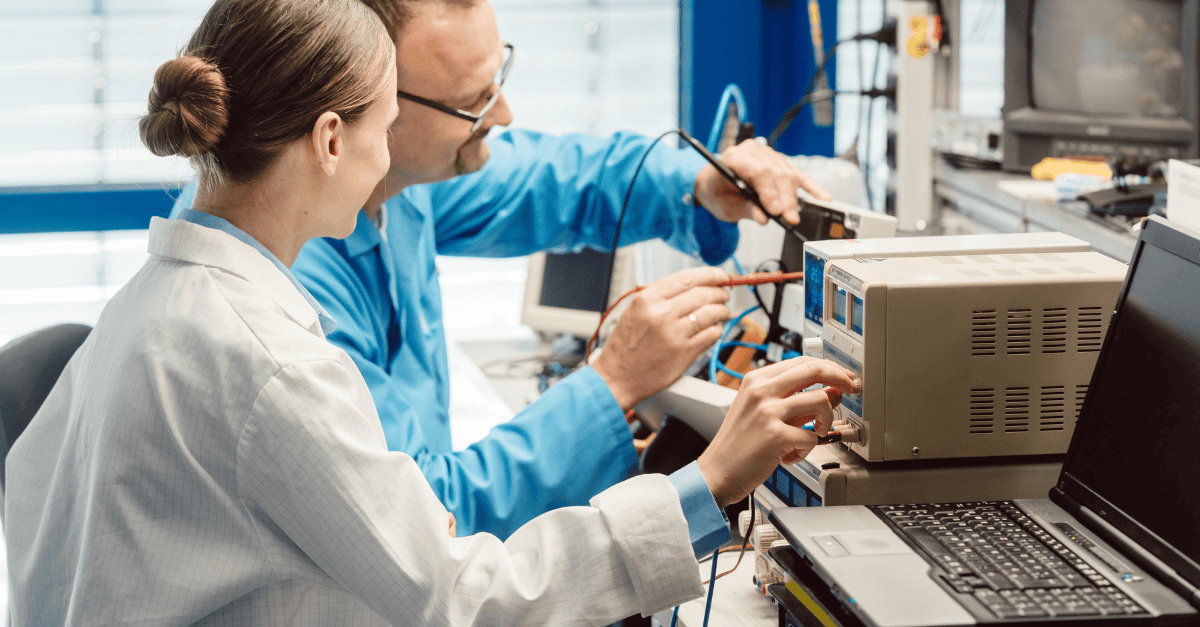
Prototyping is a crucial part of the medical device development process. A prototype represents the first tangible form of a device, transforming a concept into reality. Its primary purpose is to test both the functionality and design of the device. This makes communication between investors and the development team much easier, you have something to show, demonstrate, and physically interact with. The team also benefits, as changes can be proposed based on a real product, facilitating collaboration and speeding up development.
Prototyping is an iterative process: test, feedback, improvement, retest. Multiple iterations help identify errors that could become costly at the production stage. Prototypes are typically made from less expensive materials than the final device, minimizing the cost of repeated iterations. It is also valuable to present the prototype to the target user group at this stage. Their feedback is invaluable for implementing meaningful changes that enhance both comfort and safety. Thoroughly testing prototypes before moving to final production ensures the device is as safe and effective as possible, after all, no one wants to use a product that has not been carefully validated.
Verification ensures the medical innovation truly meets user needs.
Understanding Device Certification
There is no possibility for a medical device to be placed on the market without proper research, testing, and confirmation that it is safe for both patients and users. In the European Union, safety is ensured through legal regulations, specifically the Medical Device Regulation (MDR). Every device must meet the requirements of this regulation, and manufacturers must fully document compliance. It is important to understand that medical devices are classified into risk classes (I, IIa, IIb, III). The higher the class, the more complex the certification process and the longer it takes. Another key aspect is compliance with harmonized standards, particularly two that are essential from the outset: ISO 13485 (quality management system for medical devices) and ISO 14971 (risk management throughout the device development process).
Conformity assessment is conducted with the involvement of a notified body, an institution that audits your documentation and evaluates your company’s processes. Once a positive assessment is issued, the manufacturer can apply for the CE mark, which is a declaration that the product meets EU requirements and a prerequisite for legal sale.
It is also important to remember that certification does not end with obtaining the CE mark. Manufacturers are required to monitor the device’s safety on the market (post-market surveillance) and report any incidents. For this reason, certification should not be seen as a “final step,” but as a continuous process that accompanies the development of the device from the very beginning – from prototyping, through testing, to production and market distribution.
Final Thought
The reasons why so many MedTech startups fail are clear: this market is highly complex, involving diverse stakeholders (patients, doctors, medical staff, investors), strict regulations, financing hurdles, and the constant need to prove both safety and value. Failure often comes not from a lack of ideas, but from gaps in execution, whether it’s an underprepared team, insufficient funding, or a product that doesn’t fully address real market needs. The key to increasing your chances lies in partnership and focus. By working with an experienced technology partner like Consonance, who can take care of feasibility studies, R&D, certification, and post-launch activities, you free up time and energy to concentrate on building your business: marketing, fundraising, and growth.
Every medical innovation starts with an idea, but only those who paired vision with the right execution made it to market. Innovation alone doesn’t change lives – execution does. With the right partners and persistence, your medical idea can become the device that truly makes a difference. The next success story could be yours.